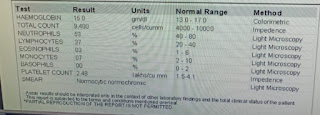
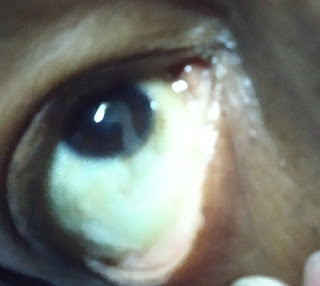
My Internship learning Experience.. Posted from I was allotted unit :4 Unit Duties OP Day We saw patients in the op. 1) As soon as the patient enters I checked for vitals. Asked about the chief complaints. Took a proper History. 2) Did the general examination and systemic examination for the them 3. Few of them came for regular check up. 4.Advised investigations 5.Advised medication as per senior order.. Few of them cases were admitted. I took responsibility for all the patients admitted in our unit. Checking out their vitals for them. Case 1) https://raveelaravi.blogspot.com/2023/06/65m-with-epitaxis-secondary-to-htn.html Patient had very low Hb: 4 mg/dL I did 2 prbc Transfuions. 2) https://raveelaravi.blogspot.com/2023/06/55-yr-m-with-paraperesis-under.htm 4) https://raveelaravi.blogspot.com/2023/06/60-yrmale-with-dyspepsia-and-typ2-dm.html Icu duties: I monitered vitals , took samble...